Millions of Americans lack access to care for asthma, COPD, and other lung conditions
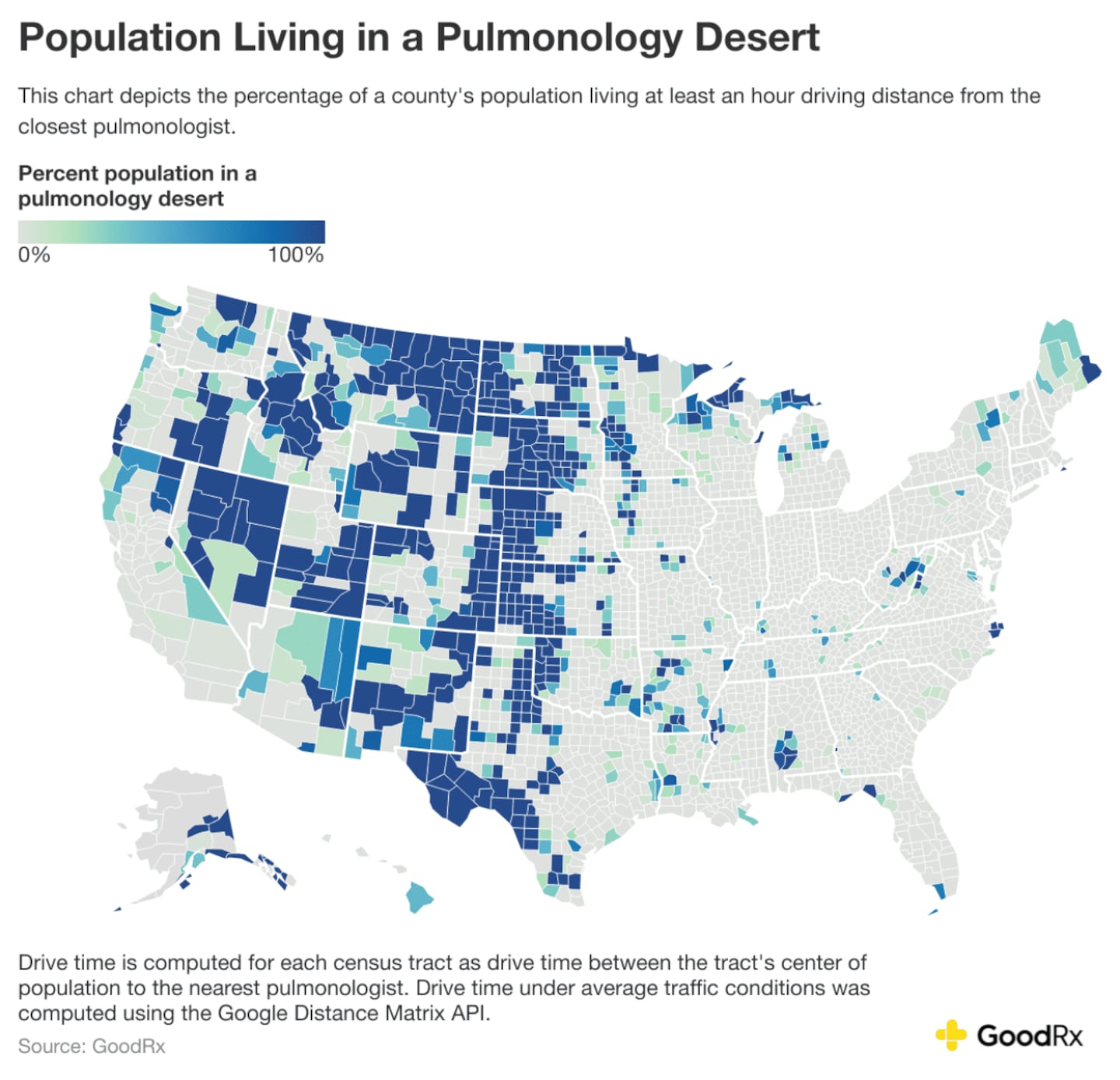
Over 5.6 million people in the U.S. live in a pulmonology desert, according to new research from GoodRx, a platform for medication savings. People who live in these deserts lack adequate access to lung care and have to drive at least one hour to get to the closest pulmonologist.
Access to a pulmonologist is essential, especially for those living with persistent lung conditions like asthma or chronic obstructive pulmonary disease (COPD). Pulmonologists specialize in diagnosing and treating diseases affecting the respiratory system. Some of these diseases can be caused by infection, inflammation, or tissue overgrowth and require long-term or lifelong treatment.
Over 16 million Americans have COPD, which is a major cause of death in the U.S. The extent of these conditions led the U.S. Department of Health and Human Services' Office of Disease Prevention and Health Promotion to list respiratory disease as an objective for their Healthy People 2030 initiative. Healthy People's goal is to increase the prevention, detection, and treatment of respiratory diseases.
Key takeaways:
- GoodRx Research finds that over 5.6 million Americans live in a pulmonology desert: a county in which more than half of the residents live at least 1 hour away from lung care.
- The number of Americans living in pulmonology deserts has increased by nearly 200,000 since 2022.
- Nevada, Montana, Utah, and much of the central U.S. have a high concentration of pulmonology deserts.
Locating pulmonology deserts
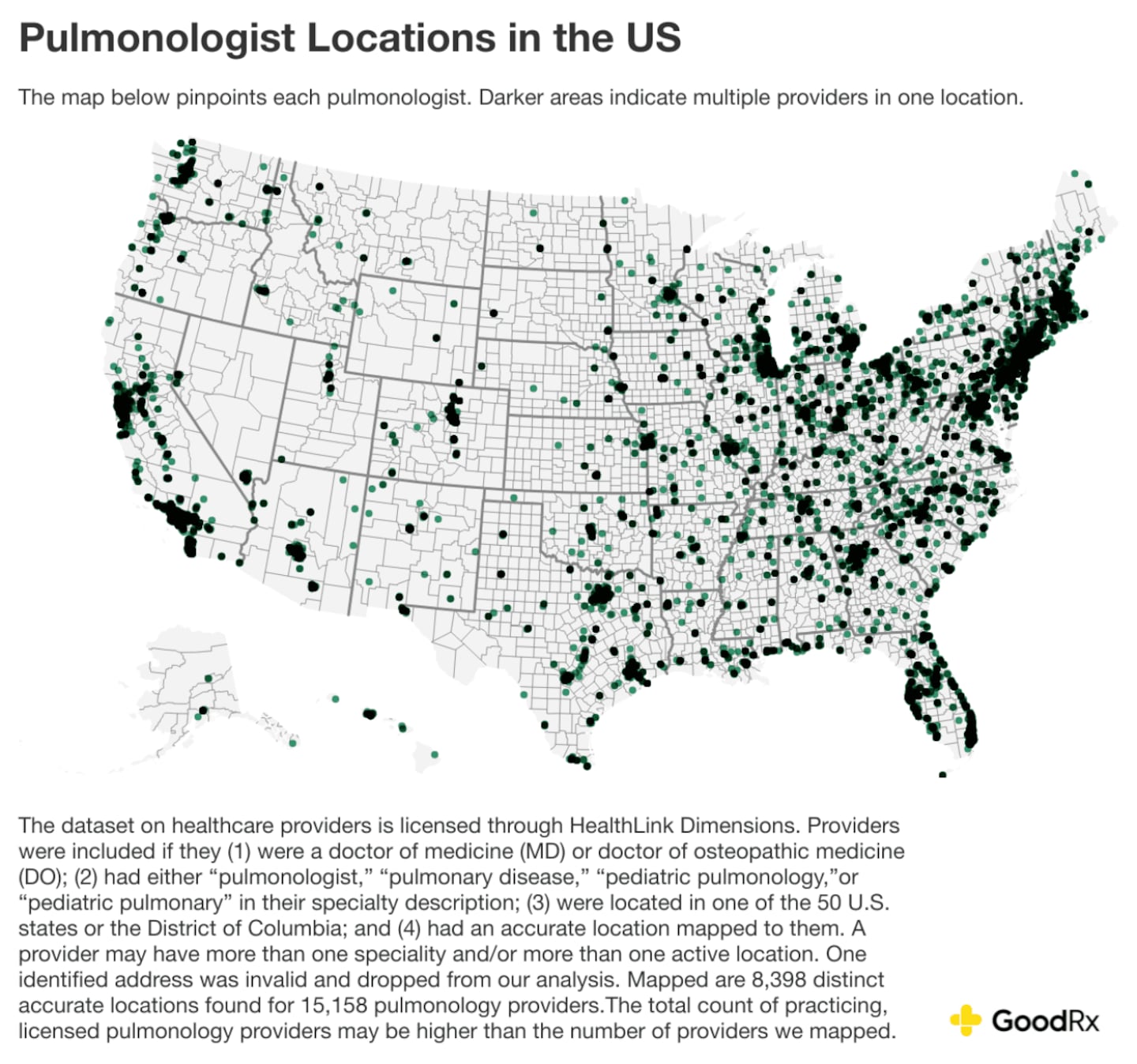
To identify areas that lack proper pulmonary care, the GoodRx Research team mapped 8,012 locations where pulmonologists practice across the country. Many locations, such as hospitals and specialty clinics, have more than one pulmonologist practicing at the same location.
GoodRx then identified counties where a majority of the population lived at least an hour from the closest pulmonologist.
Similar analyses have also used the one-hour threshold. That's because this drive time can affect a patient's ability to seek care. They may struggle to find transportation, afford the cost of transportation, or take time off work.
GoodRx uncovered 506 desert counties in total, marked in blue on the map below, accounting for over 5.6 million Americans. The counties in dark blue represent areas where 100% of the population lives in a “pulmonology desert.”
Even though there are nearly 17,000 practicing pulmonologists throughout the U.S., these healthcare professionals are dispersed unevenly across the country.
GoodRx
Living in a pulmonology desert
The majority of those living in a pulmonology desert county will need to drive at least one hour to see a pulmonologist. But GoodRx research found that many face much longer drive times, which can vary significantly by county.
For instance, the 48,000 residents in Val Verde, Texas, must drive nearly 2.5 hours to the nearest pulmonologist. That is at least five hours in the car, likely requiring the individual to take a full day off of work. In Nevada, some residents face even longer drive times. In Eureka county, Nevada (population 2,000), the closest pulmonologist is over four hours away. In White Pine and Lander counties (combined population, 15,000), the drive time is 3.5 hours.
In 2022, GoodRx pulmonology desert maps revealed a clear pattern: Many deserts are concentrated in the central U.S., specifically, North and South Dakota, Nebraska, and Kansas. And three years later, the same pattern remains. Additionally, nearly all counties in Montana and Nevada are pulmonology deserts in 2025, just as they were in 2022.
Understanding the pulmonology care gap
One possible explanation for the disparity in pulmonology access is the broader challenge of healthcare in rural areas. These states have many rural areas, where access to hospitals and primary care is already limited. And physicians often remain near their training locations, with fewer relocating to rural areas to establish and grow their practices.
Other possible explanations could be a lack of incentives for pulmonologists to practice in these areas, in addition to a lack of resources outside of large hospital ecosystems. Further, since pulmonologists often collaborate with other specialists, like cardiologists, oncologists, and rheumatologists, there may be a desire to work in closer proximity to these types of physicians.
We included both pulmonary and pulmonary critical care physicians in our analysis. However, pulmonary critical care physicians are trained to treat pulmonary patients as well as patients in the intensive care unit (ICU). So those who only practice pulmonary care are key to filling the gap for pulmonary patient care when there aren’t enough pulmonary critical care physicians available.
And there's a real need to fill the gap in lung care across rural counties. According to the American Lung Association, COPD impacts 8% of the rural population, versus 5% of urban communities. Similarly, the impact of COVID-19 has played out unevenly across rural and urban communities. While infections spiked in dense urban areas at the start of the pandemic, rural areas faced rising numbers of infections, hospitalizations, and deaths as the pandemic unfolded. As people navigate long COVID, accessible lung care remains an ongoing issue, including those in pulmonology deserts.
The bottom line
Millions of people in the U.S. live in a pulmonology desert, meaning they need to drive at least one hour to access lung care. Long drive times present a serious barrier to the ongoing care that’s often needed to manage respiratory conditions like asthma, COPD, and long COVID. Despite the unwavering demand for lung care, the number of pulmonology deserts has increased in recent years.
Methodology
GoodRx
The dataset on healthcare providers is licensed through HealthLink Dimensions. Providers were included if they (1) were a doctor of medicine (MD) or doctor of osteopathic medicine (DO); (2) had either ''pulmonologist," "pulmonary disease," "pediatric pulmonology,"or "pediatric pulmonary" in their specialty description; (3) were located in one of the 50 U.S. states or the District of Columbia; and (4) had an accurate location mapped to them. A provider may have more than one speciality and/or more than one active location. Mapped are 8,012 distinct accurate locations found for 16,763 pulmonology providers.
Drive time was computed for each census tract as drive time between the tract's center of population (based on the 2020 census) to the nearest pulmonologist. Drive time under average traffic conditions was computed using the Google Distance Matrix API. Tracts with 0 population or missing valid driving time to the nearest pulmonologist were excluded from the analysis. The percentage of a county population living in a pulmonology desert was weighted using tract population living at least an hour driving distance away from the nearest pulmonologist.
Our estimates for drive times and desert counties are likely conservative. It's probable that people will have to drive farther than we have estimated. We only mapped a tract to the closest provider, but it’s likely patients may run into issues that would cause them to need to drive to a provider even farther away. For example, their closest provider may not take their insurance coverage, may not have appointment availability due to a high caseload, or lack medical infrastructure only found in hospitals that the patient needs.
This story was produced by GoodRx and reviewed and distributed by Stacker.